Osteoporosis Risk Factors
Osteoporosis is caused by bone loss that results in an increased risk for fractures. There are two types of osteoporosis. Type I associated with postmenopausal women, 50 to 70 years old, in which estrogen deficiency is the assumed cause. Type II osteoporosis is associated with aging and assumed to be from a reduction in calcium absorption. This affects an older people over 70 years old and results more often in hip fractures. Other than calcium deficiency, osteoporosis may also occur due to physical inactivity, elevated cortisol, hyperthyroidism, and steroid medications.
There are additional risk factors for osteoporosis, such as a sedentary lifestyle, depression, chronic stress, and nutrient deficiencies. Depression and chronic stress both entail activation of the sympathetic nervous system. The sympathetic nervous system releases epinephrine, which causes a breakdown in bone matrix. Nutrient deficiencies, aside from decreasing the raw materials necessary for bone creation, can cause depression and stress.
Other than osteoporosis, caused by the thinning of the bones, the common bone and joint diseases include:
- Paget’s disease, affects the formation of bones in the body
- Osteoarthritis, affects the joints instead of the bones
- Rheumatoid Arthritis, caused by inflammation of the joints with the symptoms of painful, swollen, or deformed joints and painful and stiff movements

Bone Mineral Density
Bone strength is determined by its material and structural properties known as bone mineral density (BMD), which is used for diagnosis. However, this parameter provides information regarding the quantity of mineral in bone, which is only one component of bone strength. One of the main causes of low bone mass is family history. Research observations provide support for a significant contribution of heredity to bone density. This study conducted among 160 adult members of 40 families with familial resemblance in bone mineral density at five skeletal sites and evaluating similarities in selected life-style factors thought to influence bone density, such as physical activity, smoking, alcohol use, and diet. Adjustment of bone density for age, height, weight, and significant lifestyle or environmental factors yielded heritability estimates for the five skeletal sites between 0.46 and 0.62. That is, 46–62% of variance in bone density was attributable to heredity. However, certain conditions, medications, and lifestyle factors may account for a potentially large proportion of the non-heritable variance in bone diseases such as osteoporosis.

Elderly Bone Issues
Our bones are continuously changing and play many roles in the body including providing structure, protecting organs, anchoring muscles, and storing calcium. It is important to build strong and healthy bones during childhood and adolescence, as well as taking steps during adulthood to protect bone health.
Osteoporosis, one of the most common bone diseases, is a condition that causes bones to become weak and brittle, depends on how much bone mass we attain when we are younger and how rapidly we lose it over time. Therefore, bone diseases in the elderly can be very serious and can cause pain, fractures or even bone cancer in patients. As we age, our bone density decreases which can cause bone disease or fractures to occur.

There are some suggestions to educate a group of elderly individuals to possibly prevent bone issues:
- Treating or monitoring bone disease in the elderly can greatly decrease their risk for pain and fractures. Decrease in bone density in seniors can cause many seniors to have brittle bones even if they do not have any type of bone disease.
- Seniors should make sure that they are doing all that they can to keep their bones strong, such as getting enough calcium and vitamin D and exercising regularly because that is the best way for them to prevent bone disease.
- When exercising, it is important for seniors to make sure that they are choosing safe activities and will not cause them to fall or get hurt as this can also result in breaks or fractures. Many seniors suffer from broken bones because of falling, so they should make sure that they have an adequate assistance if they have trouble walking.
- Weight-bearing possible exercise is one of the most common suggestions for decreasing osteoporosis risk and slowing its progression. Muscles attach to bones, and when people lift weights, it puts a strain on those attachments which stimulates osteoblasts to create more bone.
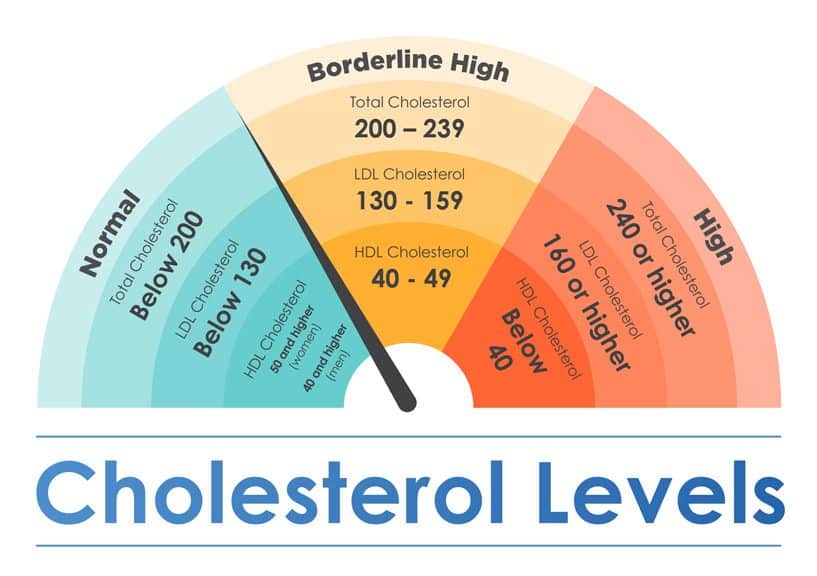
Calcium and Bone Protection
Calcium is known to prevent bone diseases and developing strong bone mineral density. For example, the Institute of Medicine advises a calcium intake of 1000 to 1200 mg a day for most adults. But we have also learned that calcium, in the form of supplements, is not risk-free. An intake of 1000 mg from supplements has been associated with an increased risk of heart attack, stroke, kidney stones, and gastrointestinal symptoms (Merz, 2015).
An analysis of reams of research — conducted by a team of New Zealand researchers led by Mark Bolland who first identified the cardiovascular risk associated with calcium supplements — concludes that increasing calcium intake has only a modest effect on bone density in people over 50. For the first analysis, they looked at more than 70 studies on the effects of dietary calcium and calcium supplements in preventing fractures.
They considered both randomized clinical trials and observational studies, and the studies varied widely in terms of numbers of participants, calcium intake, vitamin D intake, and how fractures were reported. The researchers found that neither dietary calcium nor calcium supplements were associated with a reduction in fractures.
These results are not a surprise to Dr. David Slovik, associate professor of medicine at Harvard Medical School and author of our Special Health Report Osteoporosis:
“I don’t believe that we’ve ever thought that calcium reduces fractures; it’s one part of a larger picture,” he says. You really can’t say ‘Take enough calcium and you’ll be fine.’
- ۰ ۰
- ۰ نظر